
New York State employees who are enrolled in the Empire Plan will be receiving new benefits cards for all enrollees and covered dependents.
The mass reissue of new cards began on Nov. 15 and will take approximately 35 days to complete. Cards will be sent to the mailing address on file for each enrollee.
When you receive your new Empire Plan benefit card(s), you can begin using it immediately. There is no need to activate the card before use.
It is recommended that you shred or destroy all prior cards.
If you have questions regarding the new Empire Plan benefit cards, please call the Empire Plan at 1-877-769-7447.
What’s different on the new cards
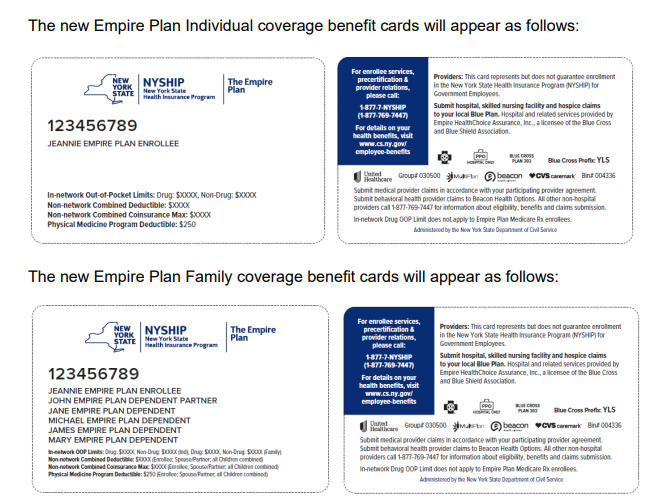
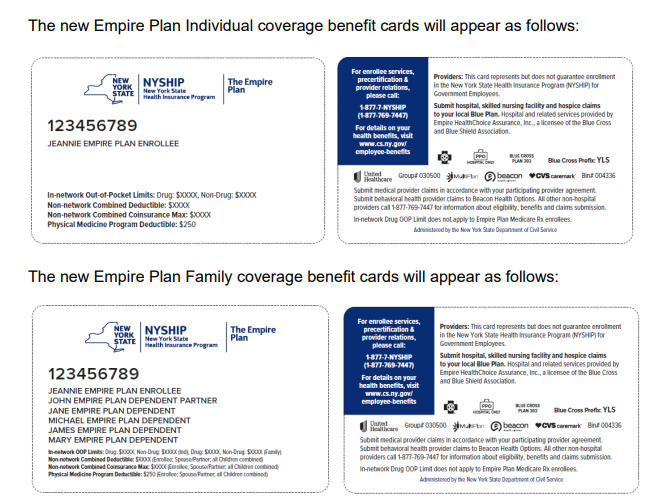
The new Empire Plan benefit cards will include annual deductible and out-of-pocket maximum information based on the enrollee’s Benefit Program. To accommodate differences in these amounts, there will be two versions of the cards (Individual and Family). Note that the in-network out-of-pocket drug maximum does not apply to Empire Plan Medicare Rx enrollees and dependents.
The cards have also been redesigned to incorporate Plan and administrator logos, the group number and bin number as well as the Department of Civil Service website.
What is unchanged
Neither your health benefits nor your nine-digit identification number (“AltID”) are changing.
The card will continue to list The Empire Plan toll-free number and other important information to aid with claims submissions. The new Empire Plan Individual coverage benefit cards will appear as follows
Additional note about HMO cards
All New York State Health Insurance Plan (NYSHIP) Health Maintenance Organizations (HMOs) will also be reissuing benefit cards for the 2022 plan year to comply with federal law. HMO enrollees should contact their HMO with any additional questions.